I’ve been living with chronic stomach pain for years—but I didn’t need to be. Steal my solution to the poor gut health that I thought was “normal” for an athlete so you can get back to training, and living, without caveats on how you fuel and function.
As a climber and long-distance runner training hard six days a week, I thought gastrointestinal distress was just an unavoidable side-effect of all the activity. After all, there’s evidence that the more blood the body directs toward the muscles, the less it can send to the digestive system. The disparity often results in compromised GI function. It’s a common concern among athletes, so I wrote off my struggles as nothing more than a small price to pay for leading a highly active lifestyle. But there came a point when I couldn’t write off the pain anymore.
Over the past year, the discomfort escalated to the extent that I had trouble eating enough to fuel my training. The food I did manage to get down sat stagnant in my stomach for hours, making me feel so heavy that I couldn’t move fluidly.
Worse yet, my recovery from training slowed down significantly as well. I went from being someone who could churn out a 20-mile-long run one morning and make links on a 5.14 the next to retaining inflammation in my body for days on end. It took more than twice as long as it once did after a training session to feel like I was ready to try hard again. I also felt like I’d lost any ability to be patient and kind with the people in my life—myself included. Given the gut-brain connection, this makes sense. There’s a direct tie between gastrointestinal distress and poor emotional regulation. In short, my physical and mental health took a serious beating.
I pride myself on having a pretty darn high pain tolerance. The willingness to push through discomfort is part of what makes me a successful athlete. When I believed that what I was experiencing wasn’t anything unusual, I simply tapped into that “grin and bear it” mentality. But when the discomfort began to have an undeniable effect on my athletic performance and my relationships, I realized that this wasn’t some commonplace complaint that I would benefit from pushing through. It was high time to figure out what was really going on.
Bacteria and the Gut
A few hundred dollars and tests later, I discovered that my gut had been terrorized by a massive H. Pylori infection. When it comes to gut health, there’s “good” bacteria and there’s “bad” bacteria. The “good” kinds support digestion and nutrient absorption while the “bad” kinds do the exact opposite. Helicobacter Pylori is part of the latter group. It’s a type of bacteria that, according to the medical team at Johns Hopkins, “can damage the tissue in your stomach and the first part of your small intestine,” which “can cause inflammation and…painful sores called peptic ulcers in your upper digestive tract.” For the first time, I cursed my beloved pain tolerance. I’d allowed this unwelcome visitor to live rent-free in my body for who knows how long out of sheer stubbornness. At least I could have faith in my iron will, if not an iron stomach.
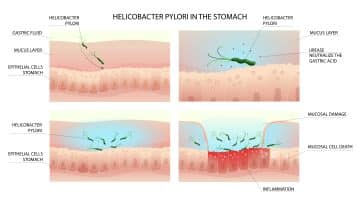
How H. Pylori bacteria wrecks havoc on gut health.
But instead of bemoaning the past, I got to work on evicting the squatter. I teamed up with a sports dietitian to create a game plan that wouldn’t require me to go on multiple rounds of antibiotics. That’s the typical treatment for H. Pylori, but one that comes with its own laundry list of side effects—many of which impact the GI system. With the amount of inflammation I was already dealing with, we decided on a longer, yet gentler, course of action.
Treatment Protocol for Gut Bacteria
That’s involved a few lifestyle changes like temporarily eliminating certain inflammatory foods (i.e. gluten), and taking five different supplements on a daily basis: GastroMend-HP (a blend of deglycyrrhizinated licorice (DGL), zinc carnosine, mastic gum, and methylmethionine sulfonium to create microbial balance in the gut), MegaSporeBiotic (a spore-based probiotic that repopulates the gut with beneficial bacteria), MegaMucosa (a blend of immunoglobulins, amino acids, and citrus polyphenols to rebuild the mucosal barrier in the gut), PhysiVāntage Redux (a blend of curcumin, tart cherry, and ginger root to decrease inflammation) and PhysiVāntage Greens (a blend of 15 various greens as well as additional pre- and post-biotics for smooth digestive function).
The first three serve the same role as a long course of antibiotics. I’ll only take them for about three months while they fight the infection and patch up my GI tract. Redux has already been a part of my regular supplement routine as a way to facilitate recovery and help with sleep. Those all seemed like no-brainers to add or continue taking. It was the daily dose of Greens that made me hesitate at first.
PhysiVāntage Greens for Gut Health
If there’s any part of my diet that I have absolutely no problem with, it’s eating enough vegetables. In fact, I probably consume more leafy greens than I really need to. The idea of supplementing with more greens seemed too superfluous to have any value. Why go to the trouble just to pee out all the excess nutrients?
That’s where I was wrong (and why it pays to have a dietitian in your ear no matter how much you think you know about nutrition). My dietitian pointed out that it’s not always about the quantity of greens but the diversity of them. A wide variety of plants translates to a wide variety of nutrients that feed all the different kinds of bacteria (of the healthy sort) in your microbiome. Simply eating enough greens in terms of quantity, then, doesn’t mean you’re getting enough variety to support healthy bacteria growth.
Besides, sometimes eating too many leafy greens in their whole food form can stress out the gut even more. It takes effort and energy to digest the roughage. When the gut is already in a state of high stress, piling on more labor might not serve the intended purpose. So, drinking rather than chewing your greens reduces the gut’s workload.
I’ve been following the full protocol for over a month now. The contrast between the life I was leading then versus now is striking. Turns out that I didn’t even know what it felt like to fuel myself without doubling over as if I’d been stabbed. I credit the combination of everything for the difference so far, but I’ve been most impressed by the one thing I was most reluctant to try.

A daily dose of PhysiVāntage Greens has been an integral part of my gut health treatment protocol.
The three gut-specific supplements actually got delayed in transit, so I started taking PhysiVāntage Greens two weeks before everything else. I’ve taken detailed notes on the whole process, and according to the timeline, the first sign of my symptoms easing off started within those two weeks after I’d started consuming a scoop of Greens first thing every morning. That’s when the breathtaking sharpness in my gut began to fade into more of a dull, background ache that occupied less and less of my attention with each passing day.
I’m looking forward to trimming down my supplement shelf in a few months. But a few habits, like a daily dose of Greens, are likely here to stay so I don’t wind up back where I started. There’s no avoiding the fact that an intense training routine does make athletes more susceptible to GI distress. But just because it’s a common complaint doesn’t mean you have to live with it. Gut struggles aren’t just uncomfortable, they’re also detrimental to our athletic performance and overall well-being. Don’t sacrifice either to suffer in silence.
Related Articles:
- Fueling for Sending with Amity Warme, Climbing Dietitian
- Performance Nutrition Through the Lens of Top Pro Climbers
- Training and Nutritional Influence on Connective Tissue Strength
- Crag Day Climbing Nutrition for Peak Performance
- Self-Care for Routesetters: Nutrition Tactics
Copyright © 2000–2024 Lucie Hanes & Eric J. Hörst | All Rights Reserved.